Legal Requests
Brand Interchange Mandate
Added required brand interchange verbiage and a physician's signature line to the Schedule III-V Refill Authorization Form, the Continuance of Schedule II Medication Therapy Form and the Authorization for Emergency Dispensing for Schedule II Medication Form for Massachusetts. The required verbiage reads:
Interchange is mandated unless the practitioner indicates 'no substitution' in accordance with the law.
Legal Disclaimer for Schedule II Refill Authorization Form
Added legal disclaimer to the fax and printed versions of the Schedule II Refill Authorization Form for Controlled Substances. The disclaimer prints on the Continuance of Schedule II Medication Therapy and the Authorization for Emergency Dispensing for Schedule II Medication. The disclaimer reads:
Disclaimer: Pursuant to DEA Code of Federal Regulations 1306.04(a) and 1306.05(f) this authorization request form may not meet the requirements of a controlled substance prescription as required by Federal and/or state law.
Refill Authorization Forms for IVR Refill Requests
When a patient requests a refill through the IVR, the system checks the drug class of the prescription to determine which refill authorization to print or fax. If the prescription is a Schedule III-V, the system prints/faxes the Schedule III, IV or V authorization form. If the prescription is a Schedule VI, the system prints/faxes the original refill request form.
Restrictions on Dispensing/Refilling Schedule II-IV Prescriptions
Added restrictions on dispensing/refilling Schedule II-IV prescriptions for California. Notice from the California Board of Pharmacy Law and Regulation:
Article 4 Refilling Prescriptions
11200. Restrictions on Dispensing or Refilling; Refill of Schedule II Prescription Prohibited
a. No person shall dispense or refill a controlled substance prescription more than six months after the date thereof.
b. No prescription for a Schedule III or IV substance may be refilled more than five times and in an amount, for all refills of that prescription taken together, exceeding a 120-day supply.
c. No prescription for a Schedule II substance may be refilled.
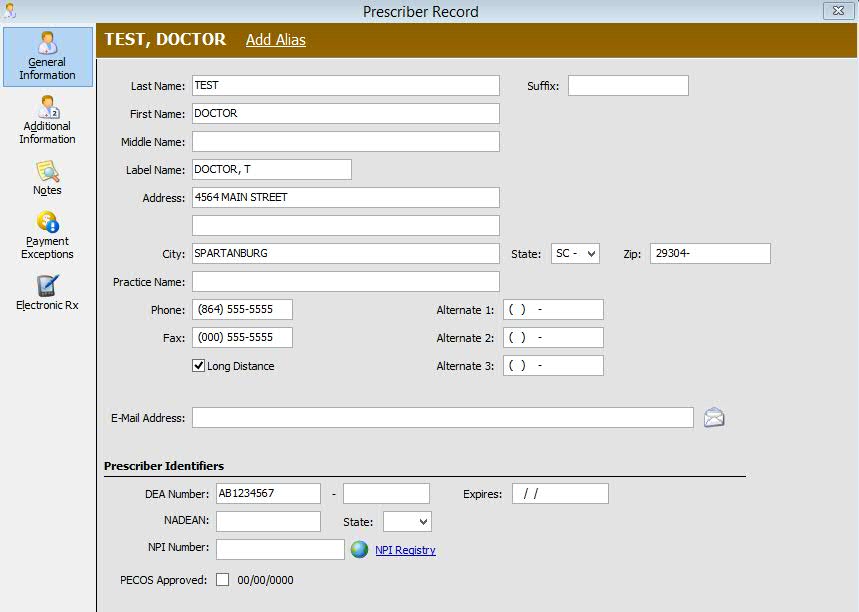
PECOS Field on Prescriber Record
Added the Provider Enrollment, Chain and Ownership System (PECOS) approved field to the Prescriber Record to indicate the doctor's verification and participation in PECOS. PECOS is for physicians and other health care practitioners to modify their provider file online and was designed so that the referring physician's credentials can be verified before Medicare claims are paid. Check this option if the prescriber is approved. Once the field is checked and the record saved, the system date automatically populates.
Added a Price Plan Message, Prescriber Not Approved for PECOS. Default = Display NO, Allow Fill YES.
Added PECOS Approved to the Prescriber File in Batch File Updates.
Quantity Prescribed (460-ET) for Schedule II Drugs
Added Quantity Prescribed (46O-ET) in billing transactions for third party prescriptions. This field is transmitted for Schedule II Drugs.
Print Drug Imprint on Compound Templates
Added the ability to print Drug Imprint information on Compound Templates with an updated label routine (Oregon).
Prevent Dispensing Opioid or Benzodiazepine Longer Than 30 Day Supply
Added the field, Max Days Supply, to the Drug Record to support the Tennessee law which no longer allows a pharmacy to dispense any opioid or benzodiazepine longer than a 30 days supply (Title 53, Section 11, Part 3 or TCA 53-11-308).
Prescription Processing
View Patient Chart When Processing an e-Prescription
Added the ability to view the Patient Chart when processing an e-Prescription. While on the Patient Record, click the View icon and select Patient Chart. The e-Prescribing sidebar remains while viewing the chart. When the chart is closed, the Patient Record re-displays.
PowerLine Data Collection for PMP Reporting
Added PowerLine functionality to collect store data based on date dispensed rather than filled date for NC PMP Reporting.
PMP Reporting for Batch Files
Added feature to allow revised and voided Prescription Records to be captured and reported in batch files for PMP Reporting (State Codes PM2 and PM4). Added Review/Update option to third party billing form programs for PMP Reporting. When this option is set to U = Update and the batch is built, the PMP submitted flag is YES on the Prescription Transaction. When selected for PMP reporting again, if the transaction is not voided, the Status Code is 01 = Revise. If voided, the Status Code = Void.
Date/Time Logging for Transferred Prescriptions
Added pharmacist/technician and date/time logging for both incoming and outgoing transferred prescriptions. The date/time will not change when a transfer is created for both incoming and outgoing prescriptions. The pharmacist/technician is auto populated when Save is selected. For an incoming prescription, this is the receiving pharmacist/technician; for an outgoing prescription, this is the transferring pharmacist/technician.
NCPDP
Added NCPDP ECL Updates:
ICD-10 Codes
Added functionality to Patient Record Medical Conditions and Rx Summary Claim Information to enter ICD-10CM Codes from a text file.
From the Patient Record, click Medical Conditions. Click ICD-10 Codes and Medical Condition Descriptions to display ICD-10 Codes. The link then offers the ability to toggle back to ICD-9 Codes. Click here to view the Patient Record Medical Conditions screen.
From the Patient Record, click Rx Profile. Select a prescription from the list and the Rx Summary displays. Click Claim Information and then click Edit Codes next to Diagnosis. Click ICD-10 Diagnosis Codes to change the display from ICD-9 to ICD-10 Codes. The link then offers the ability to toggle back to ICD-9 Codes. Click here to view the Diagnosis Codes screen.
The functionality for ICD-10 Codes is the same as for ICD-9 Codes.
Batch Processing
Added two batch views, Partially Authorized and Authorizing Payment Only, to identify batches that are not moving forward. These batches may be partially approved or frozen in authorizing payments. Partially approved batches have multiple prescriptions with some prescriptions approved and waiting for the authorization step; other prescriptions in the batch have errors or are pended. Having these views allows you to identify these batches and determine if they should be split.
Added the report, Batches Delayed in Workflow, to the Management Report menu.
Added the option to pre-authorize a high priority batch. NOTE: This function is only available for pharmacies authorized for ShipRx. This option is only enabled for batches that have been closed and are ready for pre-authorization. When the option is selected, the batch moves to the front of the pre-authorization queue.
Added the column selection, Dispensing Station, to Workflow/Prescriptions for Labeling - Batch View. This field is available for all pharmacies using Workflow.
Workflow Queue Counts
Added an option, Click for Total Counts Higher than 50 Items. If this option is checked, counts above 50 are not verified unless the pharmacy clicks on Total Item Counts. The Workflow queue stops counting if the number gets above 50 and the scans display '>50'. Click >50 to display the total count.
Workflow and InstantFill
Added the ability to InstantFill a pended prescription in Workflow. Check the option Process InstantFills on the Workflow Note window to set the option. Click Process InstantFills on the Workflow Error Resolution tool bar and any pended prescriptions in the queue that have a date and time due that is the same or prior to the current date and time due are submitted for filling.
Labels
Added a Label Routine, 759, to prevent a label from printing if the third party response has a negative adjudicated amount. The routine is 'No Label if Neg Adjud Amt.'
Reports
Third Party Billing Forms/1500 Form
The current 15A Third Party Billing Form program now prints the 02/12 1500 Form. If the Print Option Use Form 08/05 = NO, the 02/12 form prints. If YES, the 08/05 Form prints. The 1500 Form Format: Default Option Codes screen displays new options:
Changed Print Provider ID in PIN Number (33) to Print Provider ID in 32b
Changed Print Provider ID in Group Number (33) to Print Provider ID in 33b
Click here to view 1500 Form Print changes. Click here to view the 02/12 Form.
Third Party Reconciliation Reporting
A new Reconciliation File was created to contain records from Manual Reconciliation and 835 Reconciliation processing. When payments are posted to the Transaction File, a record of the payment is posted in this new file. The option, Check Number, was added to Primary, Secondary and Tertiary Carrier Manual Reconciliation. Access Systems Utilities, Reconciliation, Manual Payment Posting (Presorted) to enter the check number (up to ten characters).
The option, Check Number, was added to 835 Reconciliation if the check number is in the 835 file. When the number is in the 835 file, the user-entered check number is ignored.
Added a Third Party Billed Summary Report to the Reconciliation Reports menu. This report lists all insurance claims billed, paid vs outstanding, as well as written off amounts. This report is a combination of three reports. The first and second reports print on Page 1 and the third report prints on Page 2. Sample Reports
Third: Current Payment Received based on the new Reconciliation File
Select Options for the first report are hard coded and run from the Transaction File. When the report is selected, Report Date options display. Use this option to select the number of months to report.
Patient Cycle Rx Report
Added a Patient Cycle Rx Report to the Management Report menu. This report assists pharmacists in synchronizing all medications for a patient to have the same refill date. Having the same refill date for multiple medications limits patient trips to the pharmacy making it more likely they will continue medications on a regular basis. This report is available as a regular or enhanced report.
This report is accessed from the Management Reports menu. The Select Options are:
Patient Last Name
Patient First Name
Patient Group
The Sort Options screen does not display for this report.
There are two versions of the report - Summary and Detail.
Options for the Summary Report are:
Summary Default = NO. If the option is YES, the Summary prints. If the option is NO, the Detail Report prints.
Include Profiled = NO. If the option to include profiles is YES, profiled prescriptions print. If the option is NO, profiled prescriptions are excluded from the report.
The Summary Report lists the patient name, date of birth, home phone, prescription count, prescriber on the Rx and the prescriber phone number. The prescriber listed on the Summary is the prescriber found on the first prescription encountered for the patient.
The Rx Count is the total number of prescriptions that are not expired, not discontinued and the last fill date of the prescription is less than 180 days from the current system date.
Options for the Detail Report are:
The Detail Report lists the patient name, address, home phone, sex, date of birth and each active prescription for the patient.
The prescription information includes the drug name, SIG, prescription number, quantity dispensed, days supply, refills filled, last date filled, price, refill due date, acquisition cost, prescriber and prescriber main phone number.
The total number of prescriptions is listed at the bottom of the report.
HME Compliance Documentation
Updated NRx HME Compliance Documentation to mark only certain PCNs as eligible for HME Compliance Documentation.
Multi-Site Management and NRx
Added the ability to view a patient's central profile prior to selecting that patient in the Central Patient Scan and adding that patient to a store.
Added a new button, View Central Profile, to the Copy Patient from MSM screen. Click to view the Central Patient Profile before choosing to add them to your location. The patient may be added from the Central Patient Profile by clicking Add Patient from the Central Prescription Profile. The system then prompts whether to Copy Patient from MSM. Click YES to add the patient or NO to view the Central Patient Profile again.
Interfaces
Increased the amount of SIG verbiage to display and store on inbound electronic prescriptions from vendors. If the SIG is > 140 characters, SIG Segment 1 displays up to 250 characters (currently set to 70); SIG Segment 2 (currently set to 70) displays up to 250. Total SIG verbiage allowed is 500 characters.