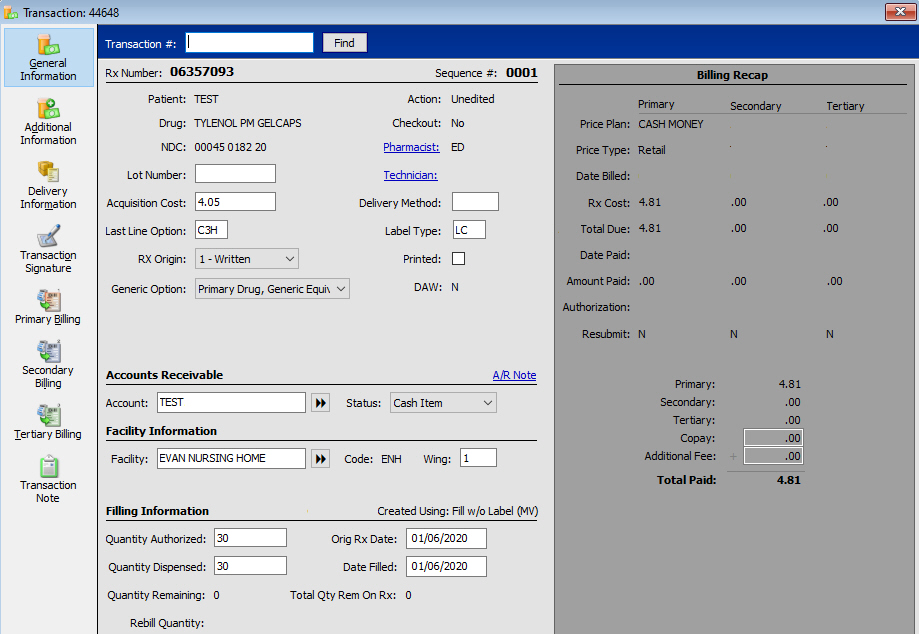
A Transaction Record is automatically created when a prescription is filled. If a prescription is filled and refilled twice, there will be three Transaction Records for that prescription. The Transaction Record is used to generate Daily and Monthly Audit Logs, Medical Expense Summaries, State Medicaid Insurance Reports and numerous other reports. Billing Recap information for primary, secondary and tertiary billing displays on the record.
There are two ways to access the Transaction File.
The first way to access the Transaction File:
1. Click ![]() on the Rx Processing Tasks menu bar. The
last transaction completed displays:
on the Rx Processing Tasks menu bar. The
last transaction completed displays:
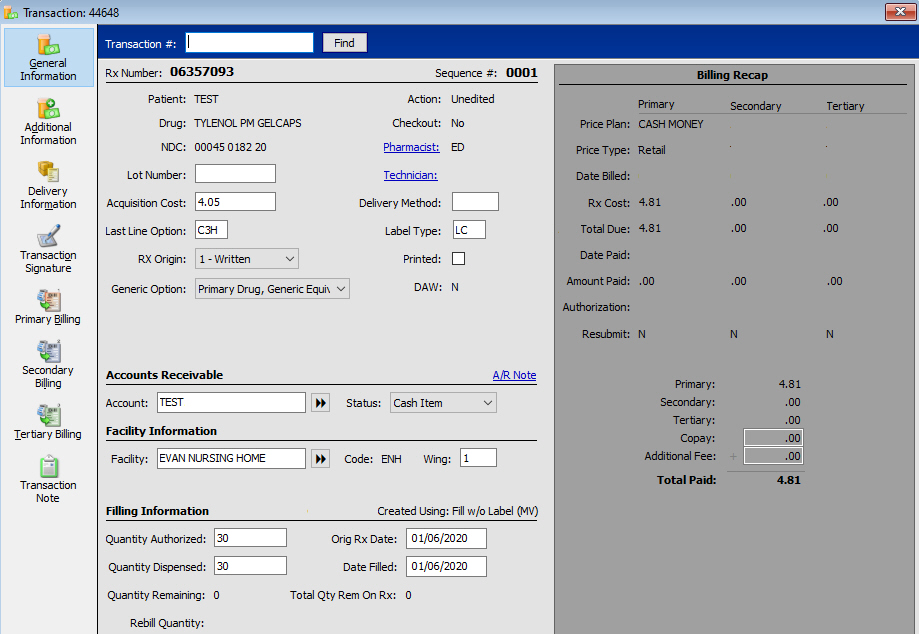
 The system-generated Fill Number field under Filling Information increases
each time a fill occurs. The exception is for partial fills; they have
the same fill number until the partial fill is completed. View
Examples.
The system-generated Fill Number field under Filling Information increases
each time a fill occurs. The exception is for partial fills; they have
the same fill number until the partial fill is completed. View
Examples.
Batch third party programs increase the fill number. The Fill Number is an Rx Transaction file report option.
The second way to access the Transaction File:
1. Access the Patient Record of the patient you want to view. Click
![]() and then double click or press the corresponding
function key of the prescription to view.
and then double click or press the corresponding
function key of the prescription to view.
2. The Rx Summary screen displays. Click ![]() and the Transaction History scan displays:
and the Transaction History scan displays:
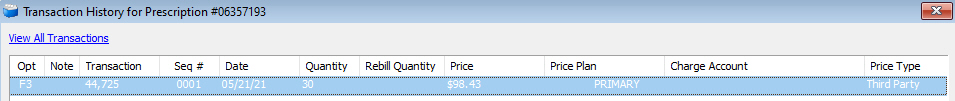
3. Double click or press the corresponding function key of the transaction to view the history for the selected prescription.
4. Click ![]() to view the Transaction
Billing History.
to view the Transaction
Billing History.
 Transaction Billing History in Store Level Options/System
must be checked to view the history.
Transaction Billing History in Store Level Options/System
must be checked to view the history.
5. The Billing Recap section on Transaction/General Information displays the Payment Plan information, as well as updated pricing information from the third party insurance.
6. Click Primary, Secondary or Tertiary Billing and the associated billing detail screen displays (Primary Billing Detail is used in the example below):
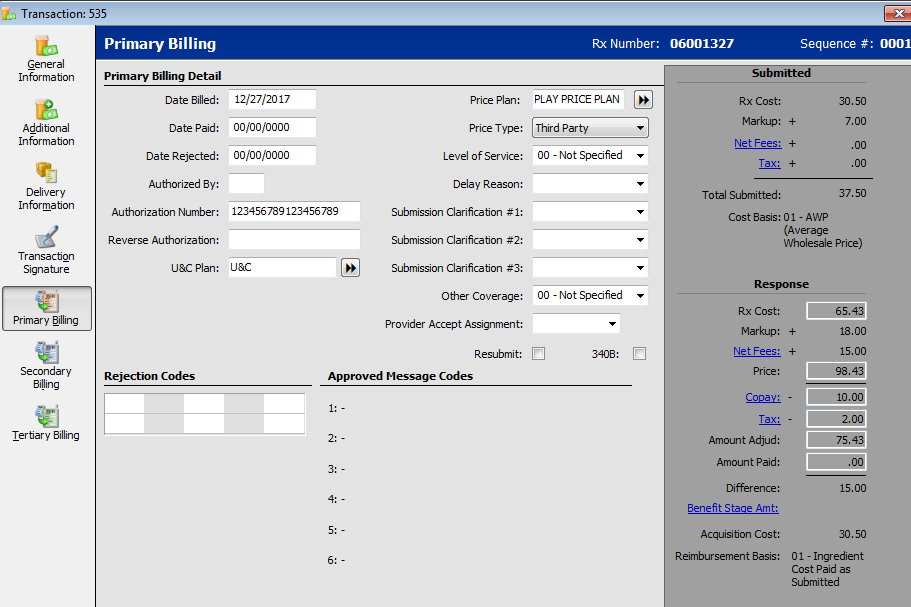
7. The following fields on the Primary/Secondary/Tertiary screens are important in the Claims Reconciliation process:
Price Plan: The third party or Medicaid Price Plan billed.
Price Type: The third party or Medicaid based on the Price Plan.
Date Billed: The date the claim was first billed to the third party/Medicaid. For electronic claims, this date is when the claim receives a Paid status.
Date Paid: The date the payment posted through Claims Reconciliation.
Amount Adjud: The amount the third party/Medicaid is expected to pay.
Amount Paid: The amount posted through Claims Reconciliation.
Return to Fill a New Prescription